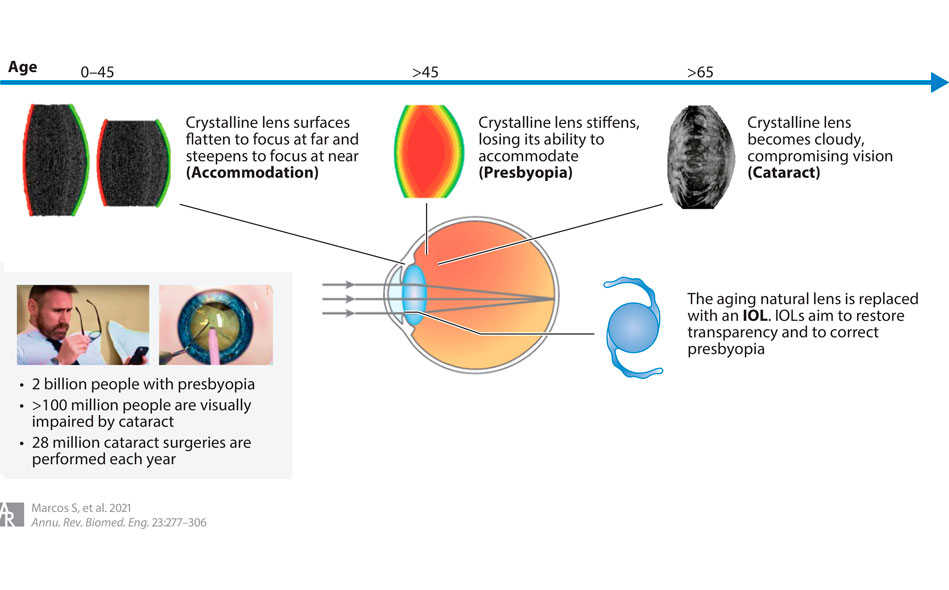
As the human eye ages, the lens hardens (presbyopia) and becomes opaque (cataract), requiring its replacement with an artificial lens (intraocular lens).
This cataract surgery is the most frequently performed surgical procedure in the world. However, although there has been a spectacular increase in the different designs of intraocular lenses available, this has not been accompanied by a sophistication in the methods of selecting the ideal lens for each patient, which is currently based on limited anatomical measurements of the eye and the surgeon's interpretation of the patient's needs and expectations.
The study
In the study, the researchers propose that the future of selecting the ideal intraocular lens for each patient will be based on three pillars: obtaining 3D images of the crystalline lens to map its opacities, anticipating the final position of the intraocular lens an once placed and to be able to know in detail the internal shape of the eye for each patient.
On the other hand, visual simulators (in which the intraocular lens designs are programmed into active elements) allow patients to experience a prospective view of the operation of the new lens before surgery and make more informed decisions about which intraocular lens to choose. .
Intraocular lenses are permanent treatments. However, patients today do not have the opportunity before the operation to know how they will see with that particular lens. The decision of which intraocular lens to implant is based on discussions of the patient's needs and expectations, but it is difficult for the patient to imagine how he or she will see with the selected lens.
Some surgeons have patients try on contact lenses to simulate what the patient can expect from certain solutions for presbyopia.
However, in a 2012 report that analyzed data from more than 17,000 eyes after cataract surgery, perfect vision was achieved in only 55% of cases.
3D optical coherence tomography
3D Optical Coherence Tomography (OCT) promises to become the preferred technique for preoperative evaluation and quantification in cataract patients prior to intraocular lens implantation.
Current scanning source optical coherence tomography methods allow 3D imaging of cataract opacities.
Furthermore, new methods of optical coherence tomography allow to obtain valuable 3D geometric and biometric data of the shape of the anterior and posterior cornea, the complete geometry of the lens, interocular distances and misalignments and, most importantly, the estimated position of the the new lens.
These data are very difficult to obtain by other methods since the lens is behind the cornea and the iris of the eye.
Simulation of the intraocular lens before implantation
A turning point in optical correction simulations was the transfer of adaptive optics (AO) technology to applications in the eye. This technology was originally developed to measure and compensate for the effects of atmospheric turbulence in astronomical observations through ground-based telescopes.
The operation is as follows: the phase map that describes the intraocular lens can be programmed into the active element of adaptive optics (for example, a deformable mirror or a spatial light modulator), and then the resulting image is projected onto the patient's eye, mimicking lens implantation. Laboratory adaptive optics systems and other alternatives to programmable corrections (such as those created with the concept of time multiplexing using tunable lenses, for example SimVis), promise to become common simulation technologies in clinics whereby patients can experience early postoperative vision with different intraocular lens designs.
Link to the article
The study is a collaboration between the Institute of Optics, the Flaum Eye Institute & The Institute of Optics of the Center for Visual Science of the University of Rochester and the Optical Laboratory of the University of Murcia